NJEA members scored a significant win in July 2020 when after nine long years of skyrocketing payroll deductions, the association negotiated with legislators to create the New Jersey Educators Health Plan (NJEHP). Members who signed up for the plan during the open enrollment that followed reaped a significant increase in take-home pay when the new plan took effect on Jan. 1, 2021.
That’s because NJEHP severed the link between the employee’s contribution and the cost of the premium, instead linking employee contribution to a percentage of salary. Better yet, the NJEHP is still valued at a platinum level plan and is similar to Direct 10 and Direct 15.
If you have not switched to the NJEHP, the next open enrollment period for districts in the SEHBP will be in October. For members in a private health care plan, please check with your district on the dates of your next open enrollment.
Of the many questions you may have concerning the NJEHP, below are the most frequently asked questions.
My district is in the School Employee Health Benefits Program. How is the NJEHP different from Direct 10 and Direct 15?
The new plan is still valued at a platinum level plan and is similar to Direct 10 and Direct 15. The notable changes are an increase in copayment for the emergency room visits that do not result in a hospital admission, the out-of-network deductible and coinsurance, and a different reimbursement schedule for out-of-network providers. For prescription drugs, there is an increase in most copayments as well as mandatory use of generic drugs when they are available.
My district has a private plan. How is the NJEHP different from my current plans?
The NJEHP is valued as a platinum level. While it is easy to compare this plan to the SEHBP program, it is not easy for the approximately 400 districts that do not participate in the SEHBP. Each non-SEHBP plan has a unique set of benefits. You should work with your local president and your NJEA UniServ field representative to determine how the NJEHP compares to your current plan or plans.
What will the premium sharing be for my health insurance?
Those plans that have been collectively negotiated in your district will continue to be offered. The premium sharing for these plans will be based on what Ch. 78, Tier 4 levels or whatever other rate has been negotiated in your contract. The premium sharing for those plans remains negotiable.
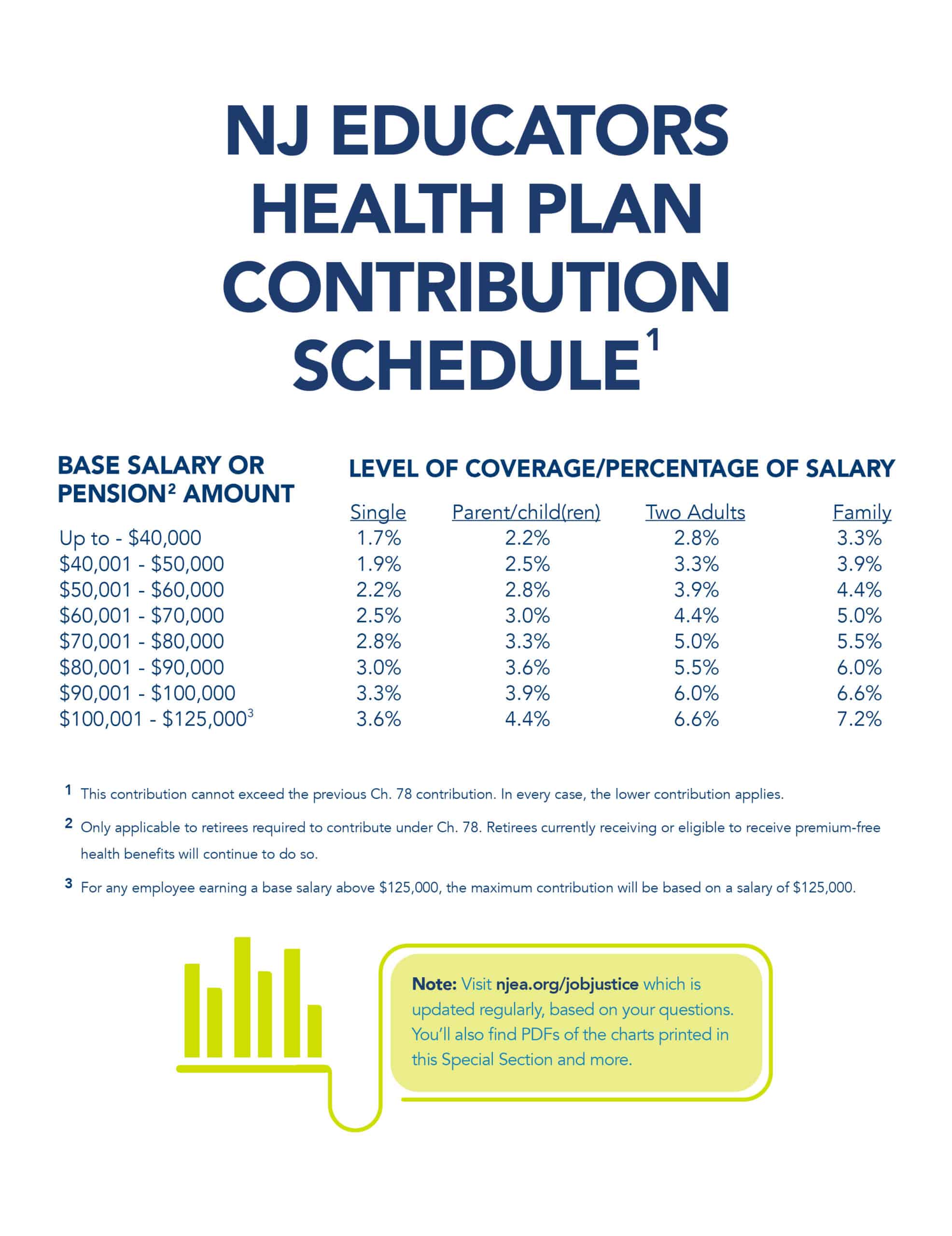
Premium sharing for the NJEHP is based on a percentage of salary set in the law. For full details, see the chart on the next page.
Can I try the NJEHP for a year?
It depends. All new employees hired on or after July 1, 2020, must participate in the NJEHP or the GSHP. Employees hired prior to July 1, 2020, have the right to move between the NJEHP and their collectively bargained insurance plans during open enrollments offered at least once a year by their employer.
How much money will I save if I participate in the NJEHP?
The law guarantees your contribution in the NJEHP will be less than or equal to what you would have paid under P.L. 2011, Ch. 78. In most cases, even where a local has negotiated a reduced premium sharing for another plan, a member will save a significant amount of money if they select the NJEHP.
Will I have to change my doctors in the NJEHP?
No. The SEHBP NJEHP will use the same network of doctors in the state and outside of the state as the Direct 10 and Direct 15 plans. If you receive your benefits from a carrier outside the SEHBP, the network must be nationally established and substantially equivalent to the SEHBP network.
The NJEHP requires the mandatory use of generic drugs (when they are available.) What if I can’t take the generic medication?
If you have tried using generic medication without success, there is an appeal process. You should contact your provider’s office to discuss it. If your appeal is approved, you will not pay the difference.
Will my prescription drugs be covered?
The NJEHP covers prescription drugs and uses a closed formulary. When there are multiple medications available to treat the same medical condition, a prescription company creates a closed formulary list, which directs prescriptions to more cost-effective, clinically equivalent medications. The medications are determined by a team of physicians and pharmacists who review all medications on a regular basis. You should consult with your doctor for alternatives if your current prescription is not covered.
The NJEHP requires the mandatory use of generic drugs (when they are available.) What if I can’t take the generic medication?
If you have tried using generic medication without success, there is an appeal process. You should contact your provider’s office to discuss it. If your appeal is approved, you will not pay the difference.